Letter to the Editor: “Proposed diagnostic volumetric bone mineral density thresholds for osteoporosis and osteopenia at the cervicothoracic spine in correlation to the lumbar spine”
by Nandong Hu, Hongye Tang, Xiao Chen (fsyy00597@njucm.edu.cn)
Proposed diagnostic volumetric bone mineral density thresholds for osteoporosis and osteopenia at the cervicothoracic spine in correlation to the lumbar spineDear Editor,
Screening for osteoporosis can be effective in reducing the incidence of fragility fractures [1]. Dual energy X-ray absorptiometry (DXA) and quantitative computed tomography (QCT) based lumbar bone mineral density (LBMD) has been used for osteoporosis detection. We recently read with great interest an article entitled “Proposed diagnostic volumetric bone mineral density criteria for osteoporosis and osteopenia at the cervicothoracic spine in connection to the lumbar spine” [2]. The authors employed deep learning methods to calculate bone mass and observed strong links between LBMD and BMD values in cervicothoracic spine. They also reported BMD thresholds for osteoporosis based on the cervicothoracic spine. Although similar studies have been done before [3,4], this study may be the first one that reported the thresholds of BMD in cervicothoracic spine for osteoporosis diagnosis. This study may supply a convenient and economical approach in osteoporosis management considering a large number of chest CT examinations everyday.
Although there are substantial value in this study, there are some concerns that remain unresolved. First, the thresholds for osteopenia or osteoporosis derived in Table 2 are based on a single vertebra, but the ACR recommends at least two vertebrae. More important, this study did not further examine the diagnostic performance of the thresholds. Second, the BMD used was also not based on dedicated phantom. The generalization of those thresholds should be validated in independent studies. Third, eight CT scanners were used in BMD measurements. It is still unknown whether different CT scanners have an impact on the data. Fourth, the thresholds of BMD in this study were obtained by substituting ACR cut-off values to the formulas. This efficiency of this method also needed further evaluation. Finally, we notice some contradictory descriptions. Figure 4 showed a high correlation for the inclusion of the degeneration and fracture groups, whereas both the results and the text show a decreasing correlation for the inclusion of the degeneration and fracture groups.
We validated the performance of the BMD thresholds of T11 and T12 reported by Rühling and colleagues in our population (30 women and 30 men, median age: 57.4 years, range: 50–69 years ), between 2021 and 2022. These people got the same multidetector computed tomography (MDCT) scan for lung cancer screening and had no spinal fractures. Synchronous QCT scans were performed to evaluate the BMD of the thoracic T11-12 and the L1-2. Osteoprosis and osteopenia were defined based on the ACR criteria. Both T11 (kappa = 0.765, p < 0.001) and T12 thresholds (kappa = 0.634, p < 0.001) had moderate agreement with ACR criteria (Fig.1).
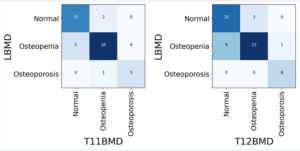
Figure 1. The performance of thresholds of T11 and T12 in identifying oteopenia (127.8 mg/cm3 for T11 and 121.0 mg/cm3 for T12) and osteoporosis (91.4 mg/cm3 for T11 and 83.8 mg/cm3 for T12). The Kappa value was 0.765 between T11 and LBMD (A). Similar results were observed between T12 and lumbar bone mineral density (LBMD) (Kappa = 0.634) (B).
In conclusion, Rühling and colleagues provided the thresholds of cervicothoracic BMD and possible value of future artificial intelligence in the diagnosis of osteoporosis. Our data showed that those thresholds had moderate agreement with ACR criteria. However, more detailed and rigorously designed studies are also needed to explore the role of cervicothoracic BMD in osteoporosis management.
